Active Learning Conversation around a 27M with Bilateral Pedal Edema and Shortness of Breath since 4 days

PGY 2-P : A 27 year old male patient presented to Kims with
C/o Shortness of breath since 4 days
Pedal edema since 4 days.
Low grade fever since 1 week
Cough since one week .
Patient was apparently asymptomatic 1 week back , when he developed fever , low grade , continuous , relieved on medication . Associated with
Cough since one week not associated with sputum ..
Patient developed shortness of breath since 4 days .. progressed from grade 2 to grade 4 .. aggreavated on walking .. and not relieved on taking rest .
Pedal edema since 4 days bilateral , pitting type from ankle to knee .!
Patient is a non alcoholic , non smoker .
Patient is a k/c/o hypertension from 2 years and on regular medication .
Patient a mason by occupation was apparently asymptomatic two years back when he was working aggressively as a Manson to build his own house ..
one night the patient had generalised weekness and fever for which he took a tab and fever was relieved for tht night
The next day morning the patient became more febrile and the patient consulted rmp doctor the next mrning .. and the doctor gave a inj for fever .. and after an hour after taking the injection , the patient became more weak and his condition deteriorated for which the patient went to a government hospital in nalgonda and was admitted and treated .. and was said by the treating. Doctors tht ..the kidney parameters are deranged ,(May be the effect was due to the injection by rmp) and patient was treated for a week and was discharged .. he was fine for the next 15 days after this and then he developed similar complaints for which he consulted a nephrologist in nalgonda .. the doctor referred him to nims hyd citing a kidney pathology and renal impairment .. the patient was then admitted at nims and was treated for 15 days and on the days of admission was told tht he had deranged kidney parameters .. and after a week of admission biopsy was performed and was told tht the patient had some kidney pathology and was given some medication for ( kidney disease) as per the patient attender .. and the patient was sent back home and was advised once a month consultation .. the patient consulted nims once a month for few months and was fine TIL the Ganesh chaturthi festival of last year .. 15 days after the festival the patient developed severe shortness of breath grade 4 and pedal edema b/l from ankle to knee .. then he was brought to Kims and was dialysed for 3 to 4 times and was in admission for 20 days .. and was put on mhd .. patient was on mhd regularly in Kims form last year and was improving and was getting admitted once in two months , for two week every time for similar complaints .and The patient came 15 back with the similar compalints .. and was admitted ...
And dialised. . And patient had complaints of cough.. and clinical patient was diagnosed with pleural effusion .. which was confirmed with chest X-ray and ultrasound and pleural tap was done and was the reports suggest clinical tuberculosis .. FOR WHICH HE WAS STARTED ON att since 2 weeks . After which the patient improved clinical and there was resolution in the serial xrays
PG Post Residency 1: Very interesting and well done history.
Where exactly did we see this patient today?
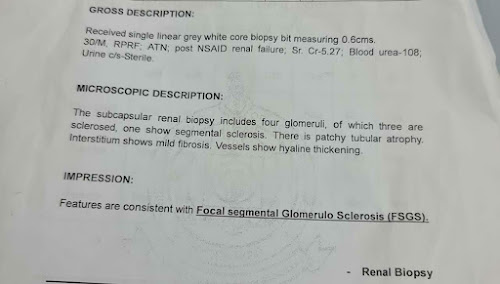
PG Post Residency 1: Would like to see the renal biopsy slide.
[7/14, 1:19 PM] PGY2-AS: Problem Representation - A 27 year old man, working as a mason involving heavy work had a background of 2 year history of Hypertension. Epidemiologically, in the absence of family history and other risk factors, secondary hypertension should be suspected, particularly in a patient whose work involved lots of exertion, which should have been protective towards BP.
In the foreground of Cough, Pedal edema and SOB allied to a backgrounds of HTN (without risk factors), my money is on CKD and hence I would think this HTN is likely secondary to a glomerular pathology. It also explains the hypertrophy on ECG. I would dig deeper and ask for family history of HTN, vascular events, a history of hematuria or frothy urine. A history of decreased urine output would help. A history of early morning facial puffiness would also help. A JVP to point the gun at the kidney and not the heart.
Worst case scenario, he may have had a URTI which led to chronic IgA nephropathy. FSGS another possibility.
[7/14, 1:21 PM] PGY2-AS: Also wouldn't mind considering an 'Athletic heart' with eccentric hypertrophy. (Is that why the Lead 1 is showing such huge R waves)
[7/14, 1:43 PM] PG Post Residency 1: He's been in your ward since few months now and is on ATT for pleural effusion that could even be due to heart failure due to hypertension and cardiorenal
[7/14, 1:44 PM] PGY2-AS: Oh this guy. He's a 30M sir and his diagnosis is FSGS
[7/14, 1:44 PM] PG Post Residency 1: Some previous discussion around him here https://m.facebook.com/story.php?story_fbid=10159953705974502&id=800154501
[7/14, 1:44 PM] PGY2-AS: His history is much different than the once presented above.
[7/14, 1:45 PM] PGY2-AS: 4 days ?!? He has been having edema and pleural effusion since December. We tapped his fluid daily.
[7/14, 1:45 PM] PG Post Residency 1: History detailed by the current nephro pg.
We are more concerned about his pleural effusion than his CRF which is just currently only amenable to replacement therapy
[7/14, 1:46 PM] PGY2-AS : It was me who prodded all the subsequent nephrology PGs to start him on ATT. I asked the faculty back in December to allow me to but they wouldn't.
[7/14, 1:47 PM] PGY2-AS: It finally came to happen in June I think and he is currently suffering the enzyme induction effects of Rifampicin with Refractory Hypertension.
[7/14, 1:47 PM] PG Post Residency 1: Good.
So you don't have any diagnostic dilemma about starting him on ATT
[7/14, 1:48 PM] PG Post Residency 1: Why can't his pleural effusion be due to recurrent heart failure or for that matter even renal failure and hypoalbuminemia?
[7/14, 1:48 PM] PGY2-AS: I did. Everyone did. He also had persistent low grade fevers. Me and rashmitha charted it for 2 weeks and saw that it did not respond to a cocktail of antibiotics. The pleural effusion too was always exudative and ADA was borderline to low.
[7/14, 1:48 PM] PG Post Residency 1 : Even if it's exudative could it still be due to uremic toxins?
[7/14, 1:50 PM] PG Post Residency 1: These and the previous renal failure with similar pleural effusion who also received att are the ones that need better platforms for shared learning
[7/14, 1:50 PM] PG Post Residency 1: Case based reasoning platforms I mean
[7/14, 1:50 PM] PGY2-AS: Yes sir. It was that case which made me incline towards TB in this one. Very very eerily similar both of them.
[7/14, 1:51 PM] PGY2-AS: No offence to anyone but this history is not even slightly close to his actual life events.
[7/14, 1:52 PM] PG Post Residency 1: Recall bias?
[7/14, 1:53 PM] PG Post Residency 1: Please share his actual events. I find this doctor data capture variation fascinating in our area of Medical cognition
[7/14, 1:59 PM] PGY2-AS: From what I remember. He developed generalized edema 2 years ago with decreased urine output. Consulted at NIMS, renal biopsy diagnosed FSGS. Dialysed him for about a week and got discharged and then started coming to us I believe. I did not see him in my first posting in May last year. Saw him in December.
One striking thing was the persistent low grade fever and tachycardia, inspite of good BP control and little respiratory distress. If I remember right, I think the HRCT we got done in December showed, Rt upper lobe consolidation with bilateral moderate to severe pleural effusion. There was, I think, mediastinal lymphadenopathy too I think.
In the BG of Immunocompromise with CKD V, with persistent low grade fevers and cough and no appetite improvement inspite of dialysis and the CT showing Rt upper lobe consolidation with mediastinal lymphadenopathy with persistent exudative taps, TB was quite high on the cards.
[7/14, 2:00 PM] PGY2-AS: We had a separate nephrology group where all the data was actively being shared. Including his beautiful fever chart. Not sure where those images are buried under now.
[7/14, 2:02 PM] PG Post Residency 1: Generally happens when you don't believe in online patient records archiving.
[7/14, 2:05 PM] PGY3-B: Sorry, but what's the cause of this FSGS?
[7/14, 2:09 PM] PGY2-AS: Primary ? Idiopathic sir ?
[7/14, 2:10 PM] PGY2-AS: And he is now having Antihypertensive resistance due to Rifampicin. Another Recall Bias I guess. The nephrology team aren't convinced with me.
[7/14, 2:12 PM] PGY3-B: I'd put that at the end of the list in such a young bloke
[7/14, 2:13 PM] PGY2-AS: Okay. Will get back with some data sir. Thanks.
[7/14, 2:21 PM] PGY2-AS: https://cjasn.asnjournals.org/content/12/3/502
Primary FSGS has several prototypical characteristics. It is probably the most common form in adolescents and young adults, although it may occur at any age. It is commonly associated with nephrotic-range proteinuria (sometimes massive), reduced plasma albumin levels, and hyperlipidemia. Histologically, it may manifest as the tip variant, collapsing variant, or NOS variant.
[7/14, 2:21 PM] PGY2-AS: Renal biopsy features that support the diagnosis of adaptive FSGS include large glomeruli, a preponderance of perihilar scars among glomeruli showing sclerotic changes, and only partial foot process effacement. Clinical features include a normal serum albumin, which is unusual in primary FSGS. A complete response to RAAS antagonism, particularly when combined with sodium restriction and a rise or normalization of serum albumin, supports the diagnosis of adaptive FSGS, although it does not exclude other forms of FSGS.
[7/14, 2:23 PM] PGY2-AS: Medication-Associated FSGS
There is a relatively short list of medications that cause FSGS. IFN-α, -β, or -γ therapy has been associated with the development of collapsing glomerulopathy in a case series of 11 subjects (89)
[7/14, 2:23 PM] PGY2-AS: Virus-Associated FSGS
Among infections, viruses are predominantly implicated in causing FSGS. HIV-1 is strongly associated with FSGS, particularly the collapsing glomerulopathy variant, although other variants are also seen (79)
[7/14, 2:24 PM] PGY2-AS: Other viruses that have been implicated in causing FSGS include cytomegalovirus, parvovirus B19, and Epstein-Barr virus, with the evidence perhaps stronger for cytomegalovirus compared with the others (reviewed in Chandra and Kopp [85]).
[7/14, 1:38 PM] MBBS UG Student 1: ECG Diagnosis : Atrial Fibrillation with LVH
Normal standardisation
Heart rate is approximately 114bpm, irregularly irregular with Narrow QRS Complex Tachycardia
Rhythm is irregularly irregular with varying RR intervals.
Left axis deviation
Absent P waves
Narrow QRS complex tachycardia, amplitude of SV1 + RV6 showing LVH (Volume Overload pattern - Tall R wave, Tall T Wave, ST elevation)
QT interval is prolonged
[7/14, 1:40 PM] PG Post Residency 1: You couldn't see the p waves 😳😨
[7/14, 1:43 PM] MBBS UG Student 1: I thought, since the QRS complexes wasn't preceded by a P wave in the beginning of L2 after the standardization box, I thought they were absent. And what we see there are T waves and not P waves.
[7/14, 1:44 PM] MBBS UG Student 1: I could be terribly wrong, pardon me, I'm still learning.
[7/14, 1:46 PM]PG Post Residency 1 : I hope you are able to see both the p and T separately in the EcG now?
[7/14, 1:46 PM] MBBS UG Student 1: But isn't the rhythm irregularly irregularly?
[7/14, 1:47 PM] MBBS UG Student 1: And there is narrow QRS complex tachycardia?
[7/14, 1:54 PM] PG Post Residency 1: All tachycardias would be that
[7/14, 1:54 PM] PG Post Residency 1: No
[7/14, 1:55 PM] MBBS UG Student 1: Oh. Looking at the rhythm strip I felt the RR intervals were not constant.
[7/14, 1:58 PM] PG Post Residency 1: It's an illusion created by the folding paper and image
[7/14, 2:31 PM] MBBS UG Student 1 : Sorry for being persistently irritating, sir. 😬I just had a few queries that I'm trying to clear up for a better understanding. The RR intervals in red are approximately 0.6 seconds and the RR intervals in yellow are approximately 0.5 seconds, so isn't the difference greater than 0.12 seconds indicating a possible irregularly irregular rhythm? And the Blue circle, is it normal to not show any P wave preceding the QRS complex? So is the Green Arrow the P wave and the Purple arrow the T Wave?
[7/14, 4:28 PM] PG Post Residency 1: 👍green p and purple t
You also got the variability of the rr interval very right.
Actually it's vital for the heart to have that much of variability.
You can read more about heart rate variability and normal variability of rr intervals and share what you learn.
You are a great active learner of your batch and please never lose your persistence 😅👍
[7/14, 4:34 PM] MBBS UG Student 1: Thank you sir. Is it normal to not have a P wave preceding the first QRS complex (as seen in the blue circle)?
[7/14, 4:40 PM] PG Post Residency 1]: Oh that was just cut off because the Ecg started after that
[7/14, 4:41 PM] MBBS UG Student 1 : 😅 Oh okay. Thank you for answering my silly questions, sir
[7/14, 4:41 PM] PG Post Residency 1 : The only way to learn EcG or for that matter anything is by asking silly questions
17/07/2020 PG Post Residency 1 :
11:00 to 12:00 ward rounds 28M with CRF hypertension started on ATT on June 23rd without PZA (?cause) and currently having severe hypertension on 4 drugs for which rifampicin stopped from today
[7/17, 11:32 AM] PGY2-P: In this prospective study, hypertensive CKD 5D patients with TB were followed after rifampicin initiation. Blood pressure (BP) was ≤140/90 mmHg with stable anti-HT requirement at inclusion. Serum amlodipine, metoprolol, and prazosin levels were estimated by high-performance liquid chromatography at baseline and 3, 7, 10, and 14 days after rifampicin initiation. BP and anti-HT requirement were monitored for 2 weeks or until stabilization. All 24 patients in the study had worsening of hypertension after rifampicin and 83.3% required increase in drugs to maintain BP <140/90 mmHg.
18/07/2020
Rifampicin was stopped yesterday, but his BP continues to spike
20/07/2020
27M continues to be breathless requiring continuous oxygen since last one week, perhaps due to his high BP, that is causing persistent fluid accumulation in his lungs due to the cardiac failure induced by his high BP, which we think is due to the drug interaction between his antitubercular rifampicin, that although stopped two days back, will still take time to wash out completely.









Comments
Post a Comment